A patients perspective
I've decided to put this page together because on looking around the internet I see heaps of rubbish, mis-information and myth out there for people who are on warfarin as an anticoagulant.Firstly - the good news
I wanted to say that managing my INR myself is incredibly simple and takes me about 5 minutes per week. Learning to use an INR monitoring machine is dead simple (a quick video provided) and (almost) any idiot can do it. If you buy strips online they cost so little that if you are an able bodied person you just couldn't consider doing it any other way.By using the Coaguchek XS I have been essentially free to travel as I wish (moved from Australia for a year in Finland, traveled to the UK and other places) and more or less unbound in any way by being on anticoagulants.
As a bonus its been really cheap, with tests costing me less than $6 per test.
In this post my main focus is on those of us who are on anti-coagulants for the fact that we have a mechanical heart valve. As I understand it there are quite a few out there who simply do not monitor their INR after their heart valve replacement, and perhaps bumble along with a fixed dose and no idea if its good or bad.
So my Valve Brothers and Sisters if you are still reading its all good news. I encourage you to go to eBay and buy a Coaguchek XS (or simmilar) get online for strips and look after your health, for your self by yourself!
In a nut shell what I do is:
- sample my blood to determine my INR
- write that down (spread sheet, but book works)
- determine if its been over time falling or rising (a graph on a SS really helps)
- make a small adjustment to my dose if needed to correct for my INR falling or rising (usually adjustment isn't needed and its better to leave it alone, more later)
Looking at the research, by following good practices (simple really) you can make life on warfarin much safer than the stats that are usually presented. Point of Care machines (like my Coaguchek) make dosing warfarin both accurate and convenient.
The rest of this post is really just here to explain more details and provide a basis for my view.
In this post I will refer to warfarin as the name of the chemical substance we take. So for those (Americans usually) who can only think in terms of product names and refer to this as Coumadin (which is actually a product name of one company) you can be clear that I am not talking about any product in particular. Calling it coumadin all the time is like saying you have a Hover instead of saying you have a vacuum cleaner when you actually own an Electrolux. I use the product called Marevan , but its unimportant to the discussion.
I thought I should also say up front that my view is that : Everything I know is subject to change based on more information. The more I learn the more I tune what I understand and how I see what I know as meaning.
I have my INR target determined by my condition, which is that I have a modern pyrolytic carbon mechanical valve. If you have other reasons for being on anticoagulants then consult with your physician as to what your target INR is and then apply that to the information below.
So, why is this here?
Essentially I was a annoyed with my INR monitoring clinic. I saw that it was essential for me to have started with them however I out grew wanting to be managed for reasons such as:- I didn't want to be fronting up for a vein blood draw fortnightly, often weekly and sometimes twice a week. It was inconvenient (as I have to go to work) and uncomfortable (as sometimes they had trouble getting blood)
- I wanted the absolute best for my health, and I became certain that only I was sufficiently motivated about things to ensure that
- I learned enough to realize I could do it better than the clinic and for less money and for less hassle
So, lets next have a ...
Quick summary
This post assumes you are already on warfarin and have been for some months. I also assume that you are not one of the small percentage of people who are having difficulties with it or having compounding problems with being on other drugs. I hope that after reading this you can stabilise your dose and stabilise your INR and reduce any possible complications ...So this in this post I say:
- keep your doses steady, by this I mean take the same number mg per day. I feel there is evidence to support that alternating high / low doses lead to increasing instability
- there is a natural swing in range of INR which will occur even with the same dose. Accept this and don't try to micro-manage it
- I have learned that nothing is fool proof because the simpler you make things the more you encourage people to be stupid. So if you can't do maths or work with numbers (like what's half of 5 + 5) and are currently with an INR management clinic, then stay with the clinic (even if you're unhappy) and just bitch about the mistakes they make (and the frustration they cause). Be comfortable in the knowledge that you'll make worse ones if you manage yourself and can't do numbers yourself.
- measure your INR consistently, getting a good sample helps (I show a video of a method I use) as does consistency of technique.
- there are many myths about INR which lead you to make wrong assumptions (and I attempt to demonstrate this with some facts), these myths perpetuate due to simplifications (aka dumbing down) and extrapolations from those simplifications.
- measure frequently (like weekly or fortnightly)
- if there is a trend which worries you, measure more often (such as again in a 3 days) to see if the trend is continuing or returning of its own accord (it may well just do that)
- adjust doses in small amounts, such as 0.5mg per day.
- split pills not average irregular doses
- don't think in weekly doses, think in daily doses
What is INR anyway?
Well INR stands for International Normalized Ratio. Wikipedia has a good summary here. Reading that one can see it boils down to a ratio (you know, like 1 over 2 is a ratio) with my clotting time (which will be longer) over the "normal" clotting time. This is of course slightly crazy as what is a "normal clotting time" ... would there not be variation in times among people?The answer is of course yes (and the details are there to be found for anyone who is interested enough to read). But for people uninterested in details I bring this up because I wish to stress a significant point:
THIS IS NOT AN EXACT SCIENCE AND THERE ARE RUBBERY EDGES TO EVERY ASPECT OF IT - SO DO NOT FRET OR OBSESS ABOUT FRACTIONS OF DECIMAL POINT.
Ok, with that (important) point out of the way lets move on... Clearly the first point in working out your INR is...
Getting Blood
Perhaps obviously when managing your INR one of the first things you need to do is get blood, to see how fast it clots. There are more or less two ways:
- the labs (which means you aren't managing your INR) use a needle and a syringe. Personally I'm no fan of "the jab" as I've had more than my fair share over (most of) my life and also only have an easy vein on my left arm. This results in frequent annoyance.
- a (finger) pin prick and use of a Point Of Care machine. This is actually becoming more common (even in hospitals) in the medical world as people begin to grasp that the devices are both sufficiently accurate and cost effective to run
So when doing this you need to follow the instructions of the device. I happen to use a Roche Coaguchek XS and it specifies 8µL or "a full haning drop". Actually getting enough blood is often not as easy as it sounds. Sure you can just give yourself a good scratch and get it, but if you do this frequently (I'll get onto that in a minute) its annoying to have what amounts to a permanent small injury on one of your fingers.
So, firstly on some mornings (I happen to test on Saturday mornings as my routine) I sometimes had trouble getting a good blood sample and would get the annoying "Error 5" displayed. This means you didn't get enough blood into the test strip and you'll have to toss the strip and try again. At $5 a hit its a slightly annoying thing to have happen ... it gets more annoying when you've blown two strips to finally get a reading with the third (meaning you've just cost $15 to check your INR).
My method is to lightly wrap a small rubber band (which I've cut to make it a small rubber strap) around my finger to act as a pressure bandage and to restrict the blood flow back up the vascular system. This means I can regularly get a reliable sized blood sample and (perhaps importantly) stay within the strict guidelines of Roche on the maximum permissible time that can pass between lancing and application (supposed to be 15 seconds, which I think is actually baseless, but that's a different post). From the Roche Coagucheck manual...
So now you know if you didn't before ...
Anyway my sample method is described in this video:
So as you can see, my method assures that:
- that you get more than enough for a good sample (and to avoid Error 5 and wasting a strip)
- do everything consistently and repeatably
- avoid milking the finger excessively (something mentioned in the manual as a no no)
- minimise the lance injury (who likes ongoing discomfort?)
- follow the 15 second rule (and preferably keep time between "ready beep" and application of blood consistent too)
Finally I would encourage everyone who is starting out taking their own INR to compare their results to a lab draw (and please, do keep which lab you go to consistent, as there is significant interlab variation). If you compare your samples to a lab make sure you always follow the same procedure, as variations of your procedure may also influence your results. When I first started I was often up to 0.8 units away from my lab. Once I'd standardised my approach I was down to less then 0.3 (which is not significant really).
Sidebar: a quick comment about lancing, always lance the side. There are a few reasons for the choosing the side:
- ask a diabetic, over time pricking the same place you damage the nerves, doing the side minimises the effect of that
- it hurts less
- the skin is thinner and so the lance does not need to be as deep
- if you need to do work later it won't be as annoying there as a finger tip
Dosing
In this post I will assume that you are already started on warfarin and have something like a stable dose (I'll discuss stable in a tic). Starting warfarin is a critical time and frequent monitoring needs to take place to ensure no problems arise and to work out your sensitivity to warfarin. Actually blood tests exist for this, and are helpful in identifying thegenes of those who need significantly lower doses. To my knowledge this is seldom done. However I digress.Being stable on warfarin essentially means that you have an INR somewhere between 1.9 and 4, even if that wanders around from time to time. I hope that by reading this post that you may be able to make some changes to how you do things and your INR fluctuations may actually reduce. In my view it would seem that to some extent achieving INR stability is made more exasperating by those who manage INR. I will present here some of what I've found and hope that it helps you.
Essentially I dose myself these days, but some people may just do their own testing, and call that into a lab or clinic who manages your dose for your (aka: tells you what to do). Personally I've found that to be a headache, although less so than when they were drawing blood and managing my INR. The reasons for this are many fold; everything from the hassle of getting in during hours I needed to be working, weird dosing advice through to overzealous micro-management of my dose and attempting to steer it.
At the end of the day you really just don't know who's at the clinic, who's keeping track of your data, what their view of this is, what dosing strategy they use, if they know diddley about it. To this end I took over my own dosing about a year after getting my mechanical Aortic valve. To be honest since then I've learned heaps and my INR is much more stable.
NOTE: I believe that if you are going to do your own dosing then you must be of the mindset to be competent to do so, be rigorous in what you do and be willing to take responsibility for yourself. If you do not feel this way, then I strongly recommend you stay under someone elses care and be a passive recipient. To me this equates to being a victim instead of in control.
So first let me present my 2013 data and I'll use that to discuss a few points. Note that each data point represents one week. If I was testing monthly (or bi-monthly as some do) I would not even see these variations. So while extra data helps to see things its important to not over react to it.

On this chart I have my INR (in blue, with the values in blue on the LHS) and my dose in mg of warfarin. There is also a red "moving average" of my INR in there too which I'll explain in a moment.
I guess that you'll perhaps see that its not "rock steady", however it sits nicely within a range of (for that period) no more than 3.4 and no less than 1.9 ... this is a pretty good range actually. This result gives me:
- an average of 2.5
- a standard deviation of 0.3
- and a score of 91% of being inside my range
I think its important to point out the language used by clinics and the misunderstanding of that by the public: when the clinics say "stable INR" they don't mean flatline (only dead people have totally steady metabolisms), essentially nobody has a "stable" INR. Rather people have INR's which will remain within a range for a given dose. Please refer to my page "the Goldilocks Dose" for a discussion of mine.
As you can see, I do make small changes to my dose, but only when I see that it is trending up or trending down. This is the reason for my having that moving average: it helps me to see this trend (in conjunction with looking at the raw data graph too). This change in trend indicates a shift in metabolism (perhaps caused by diet, perhaps by health ... it doesn't matter), and you can then re-position your dose by a small amount to optimize your outcome.
Some important points emerge from a closer look at the graph too. For instance in the earlier part of the year I was in hospital to have some surgery, there they managed my dose and took me off warfarin for a few days for the surgery. You can see that my dose went down substantially (soon to be followed by my INR). I increased my dose (from 6 to 7mg) and my INR responded rapidly. It fell a little and I thought I should increase my dose by much less at this point) and it rose again. Anyway, you can see the see saw effect happening, frequent dose changes, rapid and significant INR swings. From this I could see the significance of small changes in my dose and developed the view that: make dose changes small.
From then on you can see that my dose changes were small, in the order of ¼ a mg per day (yes, that's right I was splitting a 1mg tablet into 4 and putting that with my 7.5mg to make it 7.75mg per day). As to why I go to such lengths of consistency is because I believe that consistency is key to this.
myths
I find it interesting that people believe ideas which are mutually inconsistent. For example:- INR takes days to show the effect of a dose change
- skipping a dose will be a big problem (and why would that be if INR takes days to be effected?)
- you can work out a weekly average dose and then divide your tablets across that (so 10mg one day, 5mg the next, or something like that)
So it is in making dose adjustments using these simplifications as a basis where we cause problems
Now (being an engineer and a biochemist based science trained person) I naturally wanted to understand if there was anything that could assist me to model my INR and make predictions. That is after all why science has got us to where we are rather than witch-craft or entrail gazing. As I had been observing my data (gathered from weekly testing) I was of the view that some patterns were emerging. What I needed next was some good experimental data...
Experimental Data
Lets look at a some data that I actually took just before I went into hospital. I knew that I was going to be off warfarin for a few days during my stay (turned out that I was off warfarin for 3 days), so it provided a good opportunity to use myself as an experiment. I like graphs, as they are a really handy way to represent numbers. If you are at a point in your life where you can't manage numbers or understand them then I urge you to not manage your own INR.My actual measured INR had a gap in it because (variously) I was in surgery, then in ICU then unable to get my hands on the data from the hospital. So I do not have a reading for some days, thus you will find a discontinuity of the Measured INR. The green line was what I initially developed for my rudimentary mathematical model of how INR may behave.
The model of INR was based on nothing more than knowledge of the half life of warfarin in the body and applying general principles to it. It is not based on measurements actually got from me (which would be bloody nice to have mind you). In general warfarin is removed by our bodies at such a rate that half of what was put in is removed over 2 days: that is to say it has a half life of about 2 days. Obviously each person is different (based on well known genetic parameters actually) and each person will have variation depending on a number of factors (health, other drugs ...). Since you take an amount of the drug every day your level of warfarin in your system is a combination of what you just took, what was left over from yesterday, the day before and so on ... so for a 7mg dose this would be something like:
7.00, then 12.25, then 15.75, then 17.85 and stabilising at 19.60
Then I've simply applied a fixed scalar multiplier to the accumulated amount. This is of course assuming that the INR response to warfarin is linear (which perhaps in part of the curve it will be). So its a rubbery model, but better than nothing.
Looking at the graph you can see that green line sank to an INR of barely above 0.5 (which is probably illogical as it will not make my blood clot faster, although that's an interesting question in itself), however (of course) the trend line didn't sink as far (sinking to an INR of 1). I have found that the moving average is a helpful tool as it essentially adds simple buffering to the system (which it may in practice have).
When both my dose and then testing did resume the INR which was measured was actually quite close to the model, somewhere between the Moving Average and the Predicted INR. That it did not rise as fast as the others did, could be attributed to (for instance) a lack of responce to the 1mg increase in dose for two days. None the less it was continuing to rise where the model plateaued out.
This makes it clear that my INR dropped rapidly upon stopping the dose (which would seem obvious) which counters the "myth" that it takes days to see any change in the INR. Its a real pitty I didn't have opportunity to measure it for the whole time. For obvious reasons I'm unwilling to go off for 3 days just for data gathering. (I know, I know, where's the commitment...)
Subsequently to this I've missed a dose by accident (and more than once I may add) and have then taken readings to see what has happened. My (sorry to say) many observations of missing a dose and taking taking daily INR readings have shown that the response of INR to change in my warfarin level is surprisingly rapid.
Thus further nailing down the coffin lid of "it takes days to see any change".
So lets examine the "alternating dose" strategy briefly in this light. As we've seen INR does vary somewhat even day by day it can be observed. People look at their calendar or pill boxes (a physical version of a calendar BTW) and think, "oh well I'll just alternate my does 10mg and 7.5 mg" (I assume such alternation is because in the USA Coumadin is commonly found in doses which includ 7.5mg and 10mg
This makes sense because medical people know that most of the general public can't be trusted with numbers (return again to my advise above for the numerically challenged) and so basic arithmetic is out of the question. Combined with the fact that few people want to have more than 2 pill sized on hand and are likely to get them confused anyway (again, I refer to my numeric advise above).
They would think that their strategy of alternating doses of 10 and 7.5mg would give a value of 8.75mg per day on average ... sadly it doesn't, but I'll get to that.
So taking this alternating dose you will likely see warfarin values (and hence probably INR values) following something like the pattern in my simple mathematical model
Which shows an average dose of 8.75 *(the orange linear trendline) and an INR potential varying between 3.4 and 3.6 ... so think kid bouncing up and down on a trampoline ... you know, simple harmonic motion.
However firstly its not that simple because you probably are taking your 10mg dose on Sunday and Saturday as shown in the above graph ... of course we all know that the weeks run into each other, so that means that on Monday you've really had the dose of 10 and 10 added ... so it will actually look like this:
Notice that now after Sunday we've got a significant extra bump in it? The modelled INR line now looks far less even doesn't it...
In fact the average is now 9 not 8.75 when we consider the entire period and the overlap of the weekly roll around from Saturday to Sunday ... To do proper alternating dose you'll need to switch your starting day in your pill box from 7.5 to 10 each week, and remember that ... suddenly its not as simple as it sounds and just keeping it "steady as she goes" with a daily dose which is the same or very close to it is looking better. ... if you can add up and divide.
I'd also say this makes the other myth of taking irregular doses and averaging across the week will be OK to be another bad idea, probably based on a simplification that the response to INR is not seen within a week.
Sure, if you really want to do it then fine, however if you have occasional high spikes of INR and a bleed event don't say I didn't give you the reasons for that.
Going back for a minute to my earlier (weekly sample) years chart we can see how on occasions small dose changes occasionally resulted in rather large spikes in my measured INR? I have the view (and I've been working on the data to support this view for some time now) that such is caused by the addition of other metabolic influences which combine to push INR high. The more things that are influences the more that the situation could occur that the INR be flung even higher due to a synergy of events.
Simple harmonic motion is just up and down, but when you add another influence things get difficult to predict. Try bouncing on a trampoline with someone else. Simple harmonic motion becomes more complex.
You may not bounce as high, or you may be flung off.
You may not think that the bounce in INR is created by the bounce in the residual levels but I see evidence that it is. I've discussed above, with a number of pathologists and even endocrinologists. However despite this I have read some idiots (clinics) giving instructions to patients for even greater variance over even greater spacings: such as alternating doses of 7 and 12 or 10mg twice a week and 6mg the other days.
God only knows what will be the outcome of that one but I doubt it's stability.
As I pointed out in my other post (see post The Goldilocks Dose), I have found that even on a dead steady dose my body has variations (bounces or oscillations) in INR even when I have a continuous regular daily dose:
| dose mg | 7 | 7.5 | 8 | 8.4 |
|---|---|---|---|---|
| MAX INR | 3.19 | 3.14 | 3.64 | 3.87 |
| Average INR | 2.43 | 2.60 | 2.77 | 2.95 |
| MIN INR | 1.82 | 1.95 | 2.08 | 2.21 |
So if someone was attempting to micro manage the INR which was falling or rising based on some other cycles (and look again at the graph above to see the times when there was variation but no dose change) it could make you even more unstable. Keep a steady hand on the tiller.
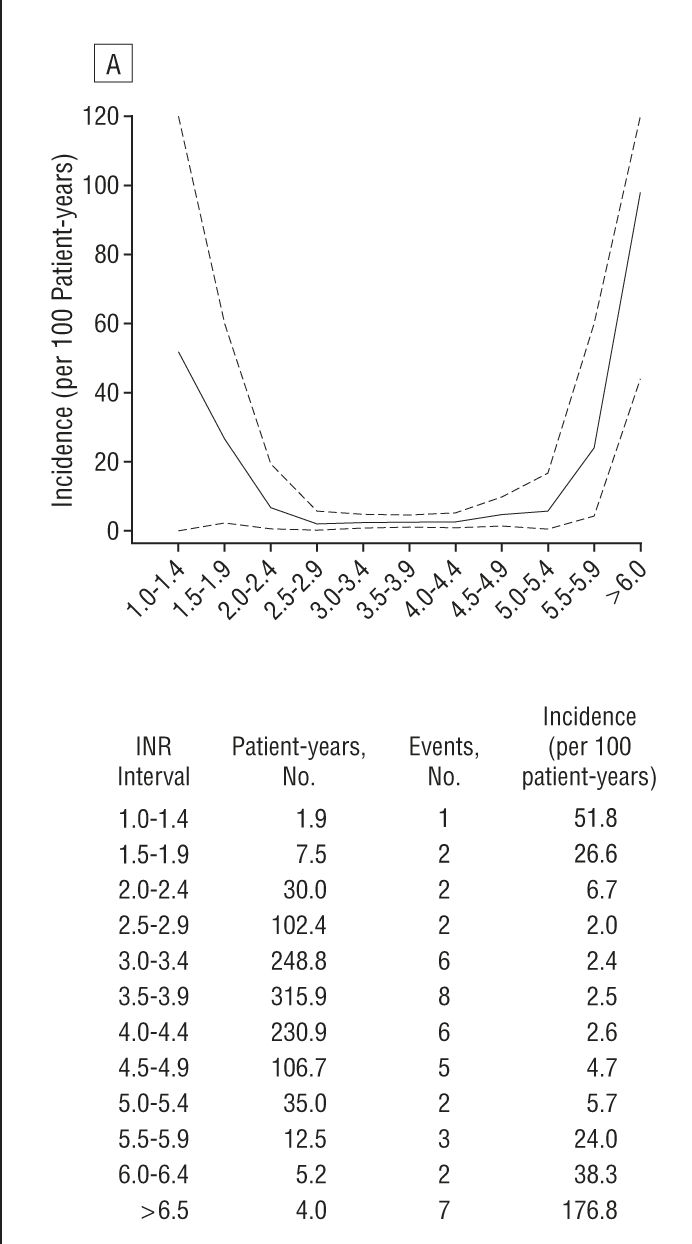
When it comes to INR range and the health issues with being too low or too high, a great resource is a study which has covered some thousands of patients and documented INR and "events". The important chart (for those of us with mechanical Aortic valves) is this one (article here)
Which shows that between 2.0 and 3.5 the number of "events" (you know, bleeds, thrombosis ... the usual stuff) is really low. Either side of that and the numbers step up. This feeds into my strategy, helping me set my bounds. Interestingly my surgeon initially recommended a range of 2.2 ~ 3 ... which sits well with the above findings...
my strategy
I aim for a target of 2.5 (which btw is the recommendation of the European Society of Cardiology for a mechanical Aortic valve, if you have a different valve you should follow the recommendations for your valve). I try to keep my variations in INR small, but know that fiddling will likely set up see saw events (making things wose). Thus I only alter dose if things are trending out of range. As I mentioned my average is 2.5 (bang on target) and my standard deviation is 0.3 ... which means that mostly I'm somewhere between 2.2 and 2.8 (if you didn't know what a standard deviation is).So now that I have set you up with much of my reasoning, I can say that basically my strategy is this:
- keep the doses regular (same dose each day)
- do not adjust dose unless you see a consistent trend down to a minimum bounds
- even then stay your hand till you know more. (I increase measurement to twice per week, this allows me to see if its sinking more still or rebounding to within bounds again)
I normally measure weekly and when I see my INR going out of bounds I do what I call an "ad hoc" measurement where I measure again on Wednesday (recalling that I measure on Saturday). This gives me the extra information to see if INR is still going low/high or has stabilised (and thus likely to return on its own).
I know that dose adjustments can set up see saw responces, so I try to alter my dose infrequently. You can see it sitting at the same level for weeks at a time in the graph above, with often only 0.25mg variations when I do change it.
I encourage you to (after reading this) again read my post on The Goldilocks Dose and review this in the light of the above some of the points I made in there. I think these two article go hand in glove, but can't work out which should be first. Specifically the points about cycles which seem to occur which result in the INR changing for the same daily dose. Also consider the idea that one can find a comfortable dose which fits within a safe range. However (as identified in that article) its possible that the natural variations may take you outside of the zone ideal zone. Naturally regular testing makes it clearer what is happening and helps you stay within range (a good thing).
At the end of the day one could take the view that I could have just sat on a dose of 7.5mg per day and been done with it. However its clear from the data that there were times when I'd have had an INR of probably close to 4 or perhaps more. If I had allowed that to happen it would actually be risky in terms of a bleed event (perhaps even provoked by a fall off my mountain bike).
So to me the answer is frequent monitoring.
Since the cost of a test is quite low I really don't mind making extra tests per year than work with some "theoretical minimum". I believe its always good to have more information than not enough. In fact not enough data leads to you not being able to understand why you had the problem.
I think that its perhaps a good time to talk about my little problem: I'm over analytical. Probably I record more data than is needed. Some people don't record as much as me or even do any analysis. Hell even I'm willing to concede that most of what I keep is only of benefit when making analysis. My Coaguchek XS stores the last 100 or so readings anyway, so if I wanted to skip back through that it shows the INR and the date.
However its no harder to keep a month of readings and graph it than it is to keep all of it. I keep my records rigorously in a spread sheet (which is backed up onto dropbox for just in case) and use that data to form the basis of my analysis and learning about myself. If nothing else it has given me knowledge and has removed the anxiety of "oh sheet, I missed a dose" ... and knowing if this is a problem or not.
Understand that your body is not a static thing and that things such as starting a new sport, stopping a sport or change of diet will alter your metabolism and you'll need to check your INR. Since you're checking weekly (see my above point on frequent monitoring) you'll pick it up quick smart anyway. If reading this has helped you to understand that change a bit more then that's a good thing too :-)
Food
Have you noticed that I haven't talked about food? Well the reason is that I've found that it makes stuff all difference (unless you eat a whole case of spinach in a sitting) and if you did start get any change to your INR you'd see that in the next weeks measurement :-) If you do see anything, work out if this is important and if its actually a consistent diet change.BTW I don't do fad diets. Instead I more or less watch what I eat ... almost all the way to my mouth so as not to get it on my shirt.
So, in short, don't stress, be happy, keep a weather eye on the horizon and a steady hand on the tiller. Make course corrections only when you are sure they're needed ...
Hopefully all this has helped you become a better navigator of your INR
Live Long and Prosper





Very well written article I have been on blood thinners for 2 years I finally had to go to another doctor to get a home tester. And your video about sticking your finger is a god send for me. It works perfectly every time.
ReplyDeleteVery interesting and useful article, with some excellent external information - thank you. I agree that consistency is important, and maintain a steady dose myself. I self-manage, testing weekly and reporting results to my AC clinic roughly monthly (on a schedule they set).
ReplyDeleteI find diet has more impact than I think you do, particularly if my consumption of leafy green vegetables varies (doubtless because of their vitamin K content), but in my research on managing INR I came across "loading doses" - a one-off increase in my daily dose of Warfarin. My normal dose is 8mg per day, and my therapeutic range is 2.5 - 3.5. If my INR drops close to 2.5 on a weekly test, I take 10mg instead of 8mg that day, and recheck 3 days later to see how it's going. So far these occasional boosts have been sufficient to restore me to a mid-range INR, and then to remain stable back on the 8mg daily dose. To be honest I don't tell my AC clinic of the changes I make - though I would do so if I ended up out of control. But in my year(ish) since the AVR I have achieved a 94% in range INR, and my 6 monthly calibration checks at the clinic of my Coaguchek XS have been within 0.2, (admittedly only 2 checks so far!) so I feel confident thus far.
But one thing I have realised since I joined the excellent valvereplacement forum is how different we all are, so maybe I am just lucky.
Hey Andy, thanks for the feedback
ReplyDeleteActually your loading dose (especially if consistently done) fits my theory. It would add to the amount of warfarin in reserve and would be slowly eroded. It may feedback into the endocrine system causing a spike in metabolism of the "toxin" (warfarin) but the amount you mention may not be sufficient to trigger that response.
I agree in full we are all a bit different, which is why I encourage all to learn about themselves in a methodical and documented way :-)
Best wishes
Wow! What an easy-to-read, and yet very informative, article.
ReplyDeleteI am on warfarin for Antiphospholipid Syndrome and struggling to get my
target INR increased from "therapeutic" to something more useful. On paper, I mean. Actual INR is up and down each week so maybe self-testing is the way to go.
All I need now is some graph paper ...
Thanks for your superb article.
I have not read anything as good on any MED sight. You are amazing. I also did this for years (decades) until I got my own meter. Then the costs rose too high. Now a nurse pops into my condo. I have a question . If she gets the irritating 5 reading she proceeds to take a second INR using the same finger with no new stick. She just uses the old one squeezing away. I voiced I felt this might not give an accurate read. She just blew me off. I called the clinic and even they did not know! (I sometimes wonder)! Perhaps you have some insight into this. And thank you for such great info. Best I have read to date. Kiki
ReplyDeleteHi
ReplyDeleteRegarding your question, what you describe is specifically mentioned to NOT DO in the Roche manual. Read the pdf and cute that to them.
As to costs, if you are in the USA and insurance is paying, then you are probably not free to do this, but strips are available online in the USA for about $5 each (by the bottle of 24) that is still quite affordable to my eyes.
If you are reading 5 then something is wrong with your management. If you are a .modern bileaflet valve with no other risk factors (like afib) then your INR should be more like 3
I would push for self management of you are able minded and can document things.
Wonderful exposition, Pellicles. Am still new to warfarin, but am keeping close track of my daily K intake and INR levels (along with a few other factors, namely daily alcohol intake and exercise), and think I'm finding a link between K intake and INR (though it's too early to say). Am wondering about the state of science on this point. Is anyone aware of good, large n studies of the connections between diet and INR levels? I haven't yet found any. George
ReplyDeleteHi George
ReplyDeleteglad it was useful information.
As to studies you won't find much because the relationship is pretty well understood, for like about 30 years. There are even such long ago established guidelines in Emergency Rooms that there is protocol for how to re-establish coagulation. Its like there are no studies done to indicate how much coal you need to burn to keep your hose warm. Its reasonably well known and there are estimates available. Only the fine tuning is needed. That's what we have thermostats for.
The fine tuning of dose is generally speaking individual and should be done with your coagucheck. This is one of the reasons why home testing is superior to lab testing, in that you yourself can get to know yourself better than any lab can.
There are known genes which if you test for them and add in other factors you can make even tighter estimates of dose ... but the reality is that its actually just FAR FAR easier to test your own INR response and adjust dose as needed (which is usually seldom).
Generally speaking you need big doses of vitamin K to make a clinically significant different to your INR , meaning that its of no significance what you actually eat (strange that clinics and word of mouth on the internet has somehow missed this detail.
I'd recommend you glance over my post on VR here
You should also keep in mind a few things:
* warfarin is removed by the body via the liver not the kidneys (specifically a Cytochrom P450 pathway)
* warfarin acts on INR by breaking down the ability to recycle Vitamin K
* vitamin K does not change the levels of warfarin in your system, it only adjusts INR by giving the mechanism more fuel (vitamin K)
So if you eat some large amount of Spinach (say you ate a Kilogram of raw spinach) then soon your INR would return to the levels it was before eating as the warfarin did its job (and assuming you kept your dose steady)
Hope that helps :-)
If you have any questions or want to discuss this in more detail, post another comment with your email address and I won't publish it but will use that to get back to you.
Happy New Year :-)
Uk based purchased a new xs machine plus kit £300 vat free because life on warfarin, Ok i set the machine up puts a strip in & loads the softclick up 1st problem the dam thing wont fire the pin = 1 x waisted strip . rings up the local chemists & they send me 100 microlets lancets , return telephone the chemists the girl thought i was on alien & could not get any sence out of her , her supurvizor rang me & it seems he cannot supply pens/applicators only the blood clinic can , Mmmmmmm ! rang my blood clinic would you believe it they use only one off disposols & dont use pens. Going to the blood clinic tomorrow to beg steal borrow some dis/lancets. This purchase of the new machine is supposed to save me stress / hassle & another thing that has come to light when i self test im supposed to telephone the results in each time yet it seems this supposed direct number he is never there to answer on the proformance so far, so common sence tells me it would be better to e mail him the results in return he can reply at his leisure same day = that seems a NO NO data protection. O the joys of modern life , why on earth would data protection be concered with my INR results the mind boggles, my own thoughts any telephone conversation is not recorded hence zero come-back if things go wrong . Cant say im a happy stress free bunny yet but things might improve ?
ReplyDeleteMisha
ReplyDeleteSorry you are having difficulty with the UK system ... it sounds like you needed better training at the start than you got. I fully understand your frustration as I went through that in Australia at first too.
I felt alone and unassisted.
But the first months are the first months and the rest of your life awaits.
Comment your email to me and I will contact you (and as you see this is moderated I will not publish that comment.
Best Wishes
So thankful that I found your article with incredible research that is so very helpful! I would appreciate your perspective on a roadblock I have encountered in my attempt to change from lab draw to coaguChek XS home monitor. After six months of using the monitor I have not been able to have the results agree with my simultaneous lab draws. Differences up to 1 point. My cardiologist is uncomfortable with that high of a difference as far as relying only upon the home monitor. Roche response is to "find a lab that uses same reagent so results will agree." Lab says "not going to happen!" My question is, Doesn't it come down to which protocol and test results are safe? If I had started with a lab that used monitors (haven't found one in my area of California USA) then my dosage would be based upon a finger stick and a home monitor would likely agree. I would be dosing from monitor results. Why is a venous draw the gold standard and therefore considered the safest? You were able to get your results from both methods to agree. Thank you for any suggestion, Donna
ReplyDelete