A post on the management of Anti Coagulation Therapy (ACT)
by
Vitamin K Antagonist (VKA) - Warfarin
I've decided to call this the rapid Dust Off INR management procedure
because you get into the risk zone and out of the risk zone as fast and as safely possible.
IMPORTANT NOTE: just like a real life Dust Off it is not without any risk (what is?) and comes with a need for experienced data driven handling of your INR; it is not for anyone who is not competent to do it.
Further this process is not intended to replace what occurs when major surgery occurs in a hospital (in case that wasn't totally obvious). In a hospital situation you must submit to their care and they will manage you (which should include restoring your ACT before discharge) they will administer heparin and supply that. So, "when in Rome..."
Background
Normally my posts are about me somehow, but this post is the work of a friend of mine who we'll call "Chuck"
About a year ago Chuck had his aortic valve replaced with a mechanical valve and began warfarin therapy. He's been an excellent manager of INR and (his words) is within range greater than 90% of the time. Yes folks that's better than clinics.
So (as eventually happens) he (like me) needed an invasive procedure where the practitioner requested that his INR be lowered to less than 1.5 for the procedure.
Now Chuck was well familiar with my perioperative management strategy for handling ACT without bridging therapy. I strongly recommend that you go over here and read about that in detail if you're not already familiar with it. The arguments and rational here depend on understanding that work.
Bridging therapy is when you
- cease one anticoagulant (warfarin),
- commence another which has a fast acting operation (heparin),
- cease that,
- have the procedure
- wait an amount of time to ensure proper coagulation has occurred (we do need this you know)
- begin heparin and commence warfarin again
- measure INR and cease heparin when INR is within therapeutic range
Its a pain not just because heparin is by injection, but because its often painful itself.
Rationale
People with mechanical valves require anti-coagulation therapy, and this is strictly about that specific application. Please read that again.
Chuck had read my (above mentioned) publication and felt that it could be improved upon (as indeed did I, but simply had not been sufficiently motivated to repeat it with improvements). Being a good student of his body response to warfarin (and naturally a good documenter of it) decided (emphasis), in consultation with his medical practitioner, to manage his INR down to 1.4 while not actually ceasing warfarin therapy.
The "
therapeutic window" (
as its called) is the range of INR where you in your situation are at the least risk of either a clot of a bleed. This is known to be between approximately INR = 2 and INR = 4 (
it depends). This information is based on
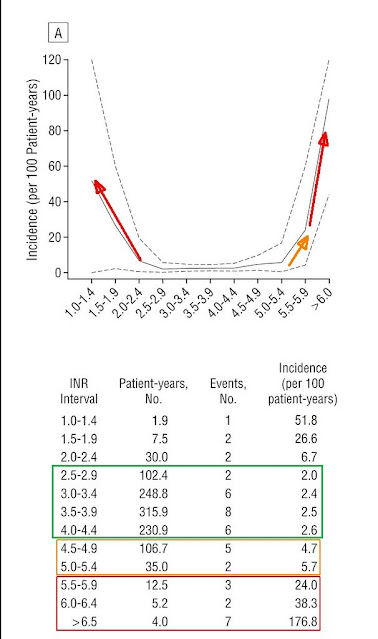
this study which I recommend you read. This figure from that summarises the risk neatly with this Figure
which I have annotated to emphasise the lowest risk regions in GREEN and the highest in RED. The numbers are pretty clear, with the range 2.5 ~ 2.9 giving a statistical probablity of 2 events per 100 patient years, even moving to 4.0 ~ 4.5 is only 2.6 events per 100 patient years. That's pretty safe and that's exactly why we call it a Therapeutic Window.
So you can see that in the range of 1.5 ~1.9 is 26.6 events per patient year, which boils down to a high chance of an event within 3.8 years.
Our intention here is to do this in far less time than that, because time is the major multiplier of risk.
Method and Data presentation
Chuck took measurements at various intervals which ranged between daily and 4 times a day. This is the sort of data acquisition which you can only get if you have your own Point of Care (POC) machine.
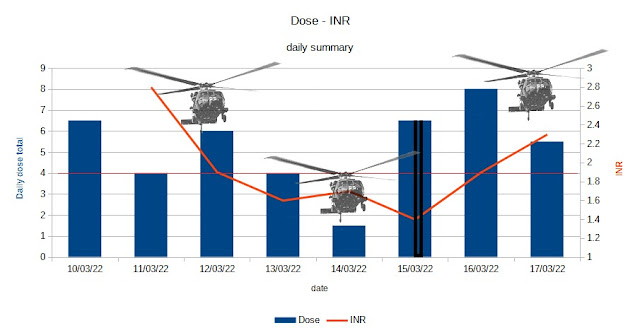
This is the summary information:
First lets identify the annotations on the graph:
- the procedure was on the 15th (black lines in the dose bar chart item)
- a red line has been added between INR 2 and 1.8 to show we are now in the hazard zone
As there was more than one dosage and more than one INR reading for some of the days I have aggregated these and taken the INR as the last INR presenting on a day and the total warfarin taken in that day as an aggregate number. The fuller presentation of data is in this chart;
This is a little more complicated, but when referring to that earlier chart. I'll leave it to the reader to read the graph.
Observations
This method enabled a a time outside the therapeutic window of just 3 days (with the 12th and 16th back within the therapeutic window. This is by any way of looking at it an excellent result.
One of the biggest issues is running out of the "antagonism cycle" where the following parts of the quite complex coagulation cascade are interfered with:
- cofactors (II, VII, IV, X)
- protein C
- protein S
The details of which the reader should look up if interested. However the point is that not only does it take time to build the right warfarin levels after you have ceased warfarin, the INR being 1 does not tell you about the levels of warfarin, but only about the levels these various factors.
By not dropping below INR 1.4 we have left the engine idling as it were. While this "engine" at idle does not produce significant power, it can be restarted again much faster. So we can be sure that some of this mechanism of antagonism of coagulation is still in place and by increasing dose we can restore the desired level of antagonism: we do not need to commence all this again from scratch.
The how and the specifics of the dose that's been used is a criteria for each person, to properly determine this you need to build up a knowledge of how your INR behaves with respect to changes in dose and changes in other factors (such as alcohol or foods). This is something that an experienced self manager will have because they have been managing themselves through a variety of cases. Additionally this method requires a rigorous approach to taking your warfarin and documenting your doses and INR.
If you are not managing yourself then this approach will require the INR manager to familiarise themselves with your particulars (not hard to do). However the literature would suggest that no INR clinic is in a position to do this for you (given that they frequently can't keep you in range > 70% of the time), meaning its best done by a competent self manager or an experienced INR manager. I guess that you can see why its not common and you've not read of it before.
Summary
This procedure is something that an experienced self manager of INR can do. It requires the careful management down of INR to a still slightly anti-coagulated state. This then allows surgeons and practitioners to undertake a procedure in the absence of significant ACT. This results in
- achieving the goal of the procedure and
- minimising the time out of therapeutic range and
- not requiring the subcutaneous injection administration of a bolus of heparin; which at the very least is uncomfortable and requires greater coordination with prescriptions and then administration of those injections
Ultimately if you are a INR self manager, and in the lowest risk category (
as defined in the above mentioned prior work of mine on this), then this procedure may be of value to you. It is intended only for
those who are on ACT primarily due to the placement of a mechanical aortic valve and who have no history of stroke. It is my view that this method should prove a helpful tool in the management of ACT around the inevitable invasive procedures we are more likely to have as we age.
Acknowledgements
I'd like to thank Chuck for the opportunity to work with him on this experiment and the generous sharing of his data.
Epilogue
Lastly I'd like to venture something I learned a long time ago, empirical observation trumps investigation into "the why" of how things work.
Theory is when we know why something should work, but it doesn’t.
Practice is when something works, but we don’t know why.
Here Theory and Practice meet: Nothing works and we don’t know why."
I prefer to go with using what I know works even if I'm not entirely sure why.