about me / introduction
I've been around in the heart valve issue for a while. I was actually more or less born into it. I was diagnosed with a heart "murmur" when I was about 6, had some early 'catheter' surgeries when I was 7 or 8, had my first OHS at about 10, which is today called something like a "valve sparing" operation, had a valve replaced with another humans (a homograft) at about 28 years old and lastly had a mechanical valve put in at about 48. These pages contain my thoughts and understandings (based on my experiences, professional medical advices and readings). So let me present my thoughts on...
The debate of: should I choose a tissue prosthetic or a mechanical prosthetic.
This is here because I take issue with the section of the "Aortic Valve and Ascending Aorta Guidelines for Management and Quality Measures" which says that there is no difference at all between valve type and survival.
I will present my view of their data (that they presented in the current guidelines) and suggest that with that the debate does not solely revolve around Tissue Valve (lack of) durability VS Mechanical Valve and anticoagulation therapy.
Discussion
So you find that you need to choose a heart valve. The news itself is probably a bombshell and you're shocked. Probably as a responce you've turned to google and dove into the internet and come up with all manner of sites and information about all manner of issues, as well as conflicting information.My advice to you is (after reading this) consider these things:
- no one via their own research will be able to learn as much as the surgeon and cardiologists you are seeing now already know. So sit back and take their advice. I know you won't do that, so here is the second bit of advice
- only read trusted sources: these are peer reviewed journals and not websites run by herbal remedy or tiddlywink vendors.
- focus your reading on working out what are questions to ask them. (Meaning your surgeon and cardiologist)
Do you trust your surgical team? Well I guess you need to trust them enough to cut through your chest, lay your beating heart bare and cut into it right? Well then you should probably trust the rest of what they say and do. However that doesn't mean there aren't divergent opinions within the medical profession and divergent reasons as to why they hold those opinions.
No matter how much you trust the skills of the team, its also important to consider issues like: patient psychology (and how that may effect the Dr's messages to you) and business models.
background
It is important to keep in mind that there is no cure for heart valve disease, only very successful options. I think it was best phased in the paper:"Prosthetic Heart Valves; Selection of the Optimal Prosthesis and Long-Term" Management " (pdf here) where it says:
Despite the marked improvements in prosthetic valve design and surgical procedures over the past decades, valve replacement does not provide a definitive cure to the patient. Instead, native valve disease is traded for “prosthetic valve disease," and the outcome of patients undergoing valve replacement is affected by prosthetic valve hemodynamics, durability, and thrombogenicity. Nonetheless, many of the prosthesis-related complications can be prevented or their impact minimized through optimal prosthesis selection in the individual patient and careful medical management and follow-up after implantation(emphasis mine)
So if you are deciding between a tissue prosthetic valve and a mechanical prosthetic valve keep clearly in mind, you are never going to go back to life as it was (ignorance can be bliss) and that you will be offered choices on how to manage. Then ask yourself the following questions:
- do you want to live: do you have a strong will to live?
- Are you a competent person able to take care of themselves (or can you learn to be)?
- Can you follow instructions and do what is needed?
The case for mechanical valves is skewed highly towards the negative in its presentation (especially in the USA) primarily because of the fear of anticoagulation therapy. Why? well I believe because people profit more from fitting you with a tissue valve than with a mechanical valve. As well people today seem to be far more anxious and frantic and short term minded. So businesses can play on that.
This is not to say there is no case for tissue valves, because there is. These are laid out in the guidelines, so if you're female and wanting to have kids, unable or unwilling to manage yourself, mentally feeble (like say intellectually impaired) or just the sort of person who has lost (or never had) capacity to take responsibility for themselves: then I recommend you put yourself in the hands of those who will take care of you and just accept what happens. Just be a Patient.
Many Surgeons only think in terms of a year or a few years, almost no older studies concern themselves with data after so 5 or 10 years. So if you get 10 years then you're out of their interest horizon. That may be perfectly good for 60 year olds who (without surgery) would not have got another 2 years. For me (at 28) it wasn't.
Its up to you ...
Arguments
On reading the latest version of guidelines for aortic valve surgery (published in 2013) titled:Aortic Valve and Ascending Aorta Guidelines for Management and Quality Measures. some questions on the decisions and data presented in this come to mind. Given that few people actually crawl through stuff like this (and just read the abstract) I thought I would. I encourage you to read the entire text to verify that you agree with what I have found in my interpretation of reading it.
This 68 page document has been 'co authored' by an impressively large committee of medical specialists. To wit

It being a committee it would stand to reason that not everyone in that list totally agrees with everything. I mean even if you have a bunch of really good friends I'm sure even finding 100% agreement on something as simple as a date for a drink will be impossible.
The first paragraph of importance to me in that document is underlined below a dearth of prospective randomised trials. meaning "we just don't have good scientific evidence". So its with interest that I read on that first page such a bold statement as:
there is no difference at all between valve type and survival

So to make this clear they didn't write:
- small difference or
- statistically insignificant difference
This is significant because it changes the guidelines primary argument that the debate revolves around tissue valve (lack of) durability VS anticoagulation. In fact I think it will become clear that anticoagulation is the key factor in managing valve disease and that avoiding it and mismanaging it can cause you more harm than good.
I thought I'd start with the age group of < 50 years old group because that's what I'm in (and the one which seems to have the greatest debates among people who are about to undergo a valve surgery).
I don't know about you, but I see differences there. What is more important is the first thing I see is 'variance' bars that are supplied at the ends of each of the data. Pericardial tissue prosthetics (I have coloured it over in green to make it clear) would seem to have the best results at first glance, however some things bear a closer look. Looking closely at Pericardial data we can see a remarkably noticeable change occurs in the survival rates at just before 10 years. Why is this so? I mean if you've ever chosen to plot a graph of statistical data you know that you get a cloud of points and its a matter of 'debate' where you put your "representative line"
The next thing that stands out to me is how big the variance range is for the Pericardial valve data. Seriously its so large as to fully encompass the best of the best and the worst of the worst. That the available data does not extend as far as Porcine valves makes one wonder how much that range will 'enlarge' as time goes by.
Next we see quite different end points. Why? It would imply that data did not exist for these valves beyond this point. I can see Mechanical prosthetic valves (red) we see a significantly longer line than pericardial, yet it does not extend to the full period. Why? Surely not from lack of data. Porcine is however plotted right out to the 15 year mark. It therefore suggests that no data exists for the other valves past those durations of time (or they excluded it).
Something is fishy with this data as this is just not right, mechanicals have a very long history and reoperation on them is much rarer. It makes (or should make) one ask questions. For example
If the mechanical valve data was plotted out to the same length of time as the porcine would it make it clearer the trend it followed gave a significant difference in survivablity.Perhaps it would ... I can only feel that the data was presented in this manner to make someone 'happy'.
Ok, looking at Allograft data (which also ends shorter), I had an Allograft in 1992, and I was part of an extensive study, so clearly that was more than 15 years before 2013 (about 21 years actually) and I was by no means the first recipient of an Allograft. This means that it is not because of data availability.
Again looking at this data what emerges is that it is hard to say you see no difference at all.
Analysis
This is interesting because it fits in with a presentation and criticism of an earlier version of these guidelines by the Mayo Clinic. I strongly urge anyone to sit through this presentation. Presented in 2010 URL , that link was originally on the Mayo site, but removed by the Mayo {presumably due to its age and it being Flash which is no longer supported, I've re-encoded it for youTube} and so that is now a link to my saved copy of the presentation) also discussed this exact topic and the presenter took issue with the 2006 guidelines which said:
His opinion on this was:
I guess that the "strong personality" (perhaps it was a corporate personality?) was again in the room for the 2013 guidelines. The difference is that this time some data was supplied at least in the form of graphs.
So lets go back to the latest guidelines and see the other graphs.
This graph (obviously) looks at patients who had operations at between 50 and 70 years of age, and once again we see that after 10 years survival of the mechanical valve cohort moving higher than the others after 10 years. Allograft did well, as well as mechanical but Porcine and Pericardial were (again) at the bottom of the chart.
Still willing to chant the mantra of "there is no difference at all between valve type and survival".
Ok, so lets go onto the data for the group who (according to conventional views) should have the least to gain from a mechanical, that is those who were 75 years of age and older at surgery.
yet it would seem looking at the data that they gained more. We see that after 10 years the mechanical valve recipients kick up substantially higher in survival rate. Sadly the Pericardial group drops to zero. Which I expect means that they died. Mechanical still has survivors at 15 years.
This is incredibly significant because for people who were operated on at over 70 years of age to get a portion of them surviving at 15 years is very encouraging. Think about that further, you're operated on at 75 (some older), and at 15 years you're 90 and still ticking fine ... would you want another OHS or trans-catheter then?
So back to the point of : there is no difference at all between valve type and survival ... well, except for that found in the data. It becomes clear that it should be restated as:
Something for the elderly in the Mayo Clinic review above is this (from my notes taken viewing to that presentation):
On the other and if the consumer (that would be you) got a single operation which gave them a valve that lasted for life where is the business sense in that?
I encourage you to read the guidelines yourself in a careful and critical way. Further I encourage you to read more from trusted sources and most importantly discuss these issues frankly with your surgeon and cardiologist.
Anyway, enough about you, think for a moment about your family.
 My wife was distraught at the thought of my surgery (more so than me), she was beside me every step of the way. She said to me in recovery that some of the happiest moments of her life were in seeing me get better every day.
My wife was distraught at the thought of my surgery (more so than me), she was beside me every step of the way. She said to me in recovery that some of the happiest moments of her life were in seeing me get better every day.
She put on a brave face, but the fact is that she was scared shitless that I would die and she would be left without me.
She was so pleased because she was so relieved. I would not want to put her through that again. If you are a reasonably healthy adult, and you choose a tissue valve you will for sure be putting your loved ones through it again.
Is that something you want to do to them?
"On the basis of these considerations, most patients over 65 years of age receive a bioprosthesis. There are no data involving narge numbers of patients that clearly show one type of or fo any individual prosthesis over another."
His opinion on this was:
"when you see something like this in a guideline then you know there was a very strong persuasive personality in the room... Because this was put in there with no supporting data ... and that person seemed to hold the day or at least last longer in the guidelines session than anybody else."He goes on to provide analysis of study after study which presented quite similar graphs to the one above.
I guess that the "strong personality" (perhaps it was a corporate personality?) was again in the room for the 2013 guidelines. The difference is that this time some data was supplied at least in the form of graphs.
So lets go back to the latest guidelines and see the other graphs.
This graph (obviously) looks at patients who had operations at between 50 and 70 years of age, and once again we see that after 10 years survival of the mechanical valve cohort moving higher than the others after 10 years. Allograft did well, as well as mechanical but Porcine and Pericardial were (again) at the bottom of the chart.
Still willing to chant the mantra of "there is no difference at all between valve type and survival".
Ok, so lets go onto the data for the group who (according to conventional views) should have the least to gain from a mechanical, that is those who were 75 years of age and older at surgery.
yet it would seem looking at the data that they gained more. We see that after 10 years the mechanical valve recipients kick up substantially higher in survival rate. Sadly the Pericardial group drops to zero. Which I expect means that they died. Mechanical still has survivors at 15 years.
This is incredibly significant because for people who were operated on at over 70 years of age to get a portion of them surviving at 15 years is very encouraging. Think about that further, you're operated on at 75 (some older), and at 15 years you're 90 and still ticking fine ... would you want another OHS or trans-catheter then?
So back to the point of : there is no difference at all between valve type and survival ... well, except for that found in the data. It becomes clear that it should be restated as:
no significant difference between valve type and survival for the first ten years.
Something for the elderly in the Mayo Clinic review above is this (from my notes taken viewing to that presentation):
The Presenter poses the question:
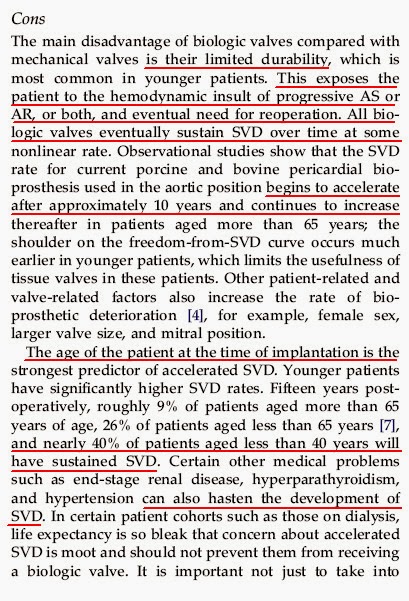
Which of course brings us to the importance of Structural Valve Degradation. Under the "Cons" section in Tissue prosthetic valves is this:
So (for patients aged less than 40 years) at 15 years 40% of these patients will have had to have their valve replaced for structural degradation. Now, lets revisit the first chart and consider these points and again examine their data. Certainly the 'trend lines' of their data does not fit the above description of Structural Valve Degradation which "begins to accelerate after 10 years and continues to increase" and that leaves "40% of patients aged less than 40 years" in SVD . So allow me put in trend lines which follow that description.
Please note that I also kept within their stated variance bars too. I also extended (in red) the mechanical data following the same trend it was following. So now looking at those data trends that are adjusted to fit their own descriptions of the data we see even more significant variance in "late survival" than before.
Actually it will only look worse for this (for tissue prosthetic valves) if you are female, and or have a larger valve size and or you have hypertension.
hmmm ....
You can find people who have had mechanical valves implanted once and 30 years later they're ticking along fine. With no other surgery required ... often with no hassles at all. You can not find that in any person with a tissue valve.
So with the choice of a tissue valve in mind lets move on to the inevitable point ...

So, if you get an infection while you are in hospital then the mortality rates are not what I would like to see for myself. It is also very interesting to look at the costs associated with these, seen over in the second last column. Seems to be good business for US hospitals (who after all in the main take people who pay).
Ok, lets look at where these infections are commonly had:
so the largest slice of infections after cardiac surgery (in this data set) is at the surgical site. And from above there is an uncomfortable level of mortality associated with an infection.
The alternative of course is to not have a second surgery, which of course means considering a Mechanical valve. Lets now have a quick look the mechanical valve issue of (insert Hammer Horror music) anticoagulation.
Since you're still reading then its clear you are interested in alternatives. As discussed, the first page of that report says:
...there is no difference at all in late survival and thus the debate revolves more around valve durability and anticoagulation.
Since we have looked at late survival, then looked at valve durablity, lets now look at anticoagulation.
The main argument against mechanical valves is the risk of thromboembolism and of bleeds and the requirement for anticoagulation.
This is the boogy man which surgeons who advocate tissue valves and serial redo operations bring out to scare you. Frequently this is portrayed as being a horror story, yet strangely it seems that its only a "known problem" among those who are not on it.
Currently Warfarin (brands like Coumadin or Marevan) is the "Gold Standard" for management of Anticoagulation therapy. It is a "narrow therapeutic range drug" which (like sleeping pills) work well with just the right dose: will do nothing if too little and will hurt you if you take too much.
Almost every case of warfarin anxiety I read about in forums about heart related issues follows the same pattern, that is:
For instance some advice I saw recently posted on a forum for heart valve patients.
The medical facts are that if you learn to manage your dose yourself (just like diabetics do, you will test and maintain an INR range)and use a machine (and there are a few on the market) to monitor your INR you will be in a much safer situation than if you rely on a clinic (data presented in a moment below). Yet in the USA the medical establishment (including the medical insurance companies) prefer you to attend a clinic which will most likely use exactly the same machine you would buy yourself (for about $500).
The money facts are that warfarin is a very low price drug (people in the US even buy it at Cosco) and self management is also very cheap. Clearly there is no money to be made in encouraging people down that path. Interestingly the best possible outcome for you is also the cheapest outcome for you.
But its important to remind you that choosing a tissue valve will not mean you are free from anti-coagulation therapy. There is a chance (especially if you are elderly you will be prescribed it for other reasons such as atrial fibrillation).
So (in my view) without mitigating 'co-morbidities' (meaning you're a regular healthy adult), get a mechanical, maintain your INR yourself and live long and prosper.
The risks of taking warfarin are of a bleed or a thromboembolism (clot leading potentially to a stroke).As is stated in the medical literature (and even in this report) the decision of Tissue or Mechanical comes down to balance of choice of tissue valve and its required reoperation or mechanical valve and anticoagulation therapy.
It is this spectre of anti-coagulation therapy which is rattled out by some surgeons (who is it doing the operation again btw?) , with suggestions that anti-coagulation may be as risky as reoperation.
Ok, firstly go back up and re-examine the data on infections ... then consider that the worst possible results from anti-coagulation therapy come from mismanagement of INR. The data on events being poor comes primarially from the results of people who are managed by a clinic rather than who self test. The effective management of INR is not in itself rocket science. Yet the medical system in the United States (where this report comes from) seems to frown upon self testing. This is despite a rather large and growing body of evidence that Patient Self Testing is more cost effective and yeilds better results.
Studies have shown that Patient Self Testing reduced the bleed complications from 11% to 4.5% and Thromboembolic events from 3.6% to 0.9%.
Yet Tissue prosthetic valves are not free from Thromboemolic events nor are the patients free from bleed complications. The article suggests that:
So the risk of Thromboembolic rates for Tissue prosthesis is greater than that for well managed INR and Mechanical valves.
On the subject of structural degradation of Tissue prosthetic valves with age The article suggests that:
So now, how well does the argument against anticoagulation stack up to you?
With modern western life expectancy as it is (assuming you are 60 or less you have another 20 or more years), why on earth would you choose a tissue prosthetic when you are clearly setting yourself up for another operation in the later years of your life?
Well, one of the reasons I typically read (on heart discussion forums) is that "I want to get over this and go back to my life as it was". Well guess what? Your life will forever be changed by this process (for a start you're alive) and it is generally much better to take the wake-up call and use this as an opportunity to see your life differently. Is taking a pill every day so onerous? Does it make you feel older? Is denial of this worth that much to you?
Of course there are clinical reasons why you may need to choose a tissue prostheses (such as the desire to get pregnant {although I'd have thought that to be reduced in women over 60Yo})
With respect to the initial surgery, the choice of a mechanical valve can make the surgery easier for the surgeon the document states:
Currently available mechanical aortic valve prostheses have several advantages

some things stand out in a quick glance:
Lets look at those numbers in another (perhaps clearer) way.
 This means that over 80% of valves sold to 'consumers' in the USA are of the type that will need replacement. In fact its quite probable that some of the valves sold in 2011 were for replacement. Since its quite rare to replace a mechanical valve selling more tissue valves gives greater possibility for then selling another tissue valve. Repeat business is good for business.
This means that over 80% of valves sold to 'consumers' in the USA are of the type that will need replacement. In fact its quite probable that some of the valves sold in 2011 were for replacement. Since its quite rare to replace a mechanical valve selling more tissue valves gives greater possibility for then selling another tissue valve. Repeat business is good for business.
Looking at the data sales of valves gives rise to something like $435,716,947 in valves alone. Think of the extra revenue generated in hospital treatments.
That's quite an industry.
"So why is that that tissue has higher mortality than mech?"
His view is that the reason for mortality increase is two part
1) reoperation risks
"its not true that the risks of reoperation are the same as the first operation."
"if somone tells you that run don't walk the other way"
2) this is a little more complex:
case a: 77 yo had severe heart failure. It could be said that this was
'Gods hand' for 77 year olds. Its not true that tissue valves don't
thrombose, they do. If not identified it can be confused with heart
failure. Patient is now anticoagulated. This patient would have died for lack of diagnosis of thromboembolism. A diagnosis overlooked because of the pervasive medical view "tissue valves don't thrombose.
case b: another patient 56yo (an MD) had neglected aortic regurgitation
(EF was21%) he also had rejected a mechanical and wanted a tissue
"because he's too young and active for a mechanical"
* reoperated at 2.5 years is now anticoagulated
case c: another patient 22yo had a tissue (wanted a family) and came back 3 years later with
thrombosis of the tissue valve.
* patient repoerated at 3 years and now antiocoagulated
Which of course brings us to the importance of Structural Valve Degradation. Under the "Cons" section in Tissue prosthetic valves is this:
So (for patients aged less than 40 years) at 15 years 40% of these patients will have had to have their valve replaced for structural degradation. Now, lets revisit the first chart and consider these points and again examine their data. Certainly the 'trend lines' of their data does not fit the above description of Structural Valve Degradation which "begins to accelerate after 10 years and continues to increase" and that leaves "40% of patients aged less than 40 years" in SVD . So allow me put in trend lines which follow that description.
Please note that I also kept within their stated variance bars too. I also extended (in red) the mechanical data following the same trend it was following. So now looking at those data trends that are adjusted to fit their own descriptions of the data we see even more significant variance in "late survival" than before.
Actually it will only look worse for this (for tissue prosthetic valves) if you are female, and or have a larger valve size and or you have hypertension.
hmmm ....
You can find people who have had mechanical valves implanted once and 30 years later they're ticking along fine. With no other surgery required ... often with no hassles at all. You can not find that in any person with a tissue valve.
So with the choice of a tissue valve in mind lets move on to the inevitable point ...
Your next surgery
Now lets do something different to the usual analysis of "how risky is a redo surgery" (which does contain more risk than the initial surgery) and that is the subject that surgeons hate to talk about: Surgical Infection rates.
So, if you get an infection while you are in hospital then the mortality rates are not what I would like to see for myself. It is also very interesting to look at the costs associated with these, seen over in the second last column. Seems to be good business for US hospitals (who after all in the main take people who pay).
Ok, lets look at where these infections are commonly had:
so the largest slice of infections after cardiac surgery (in this data set) is at the surgical site. And from above there is an uncomfortable level of mortality associated with an infection.
The alternative of course is to not have a second surgery, which of course means considering a Mechanical valve. Lets now have a quick look the mechanical valve issue of (insert Hammer Horror music) anticoagulation.
Since you're still reading then its clear you are interested in alternatives. As discussed, the first page of that report says:
...there is no difference at all in late survival and thus the debate revolves more around valve durability and anticoagulation.
Since we have looked at late survival, then looked at valve durablity, lets now look at anticoagulation.
The main argument against mechanical valves is the risk of thromboembolism and of bleeds and the requirement for anticoagulation.
This is the boogy man which surgeons who advocate tissue valves and serial redo operations bring out to scare you. Frequently this is portrayed as being a horror story, yet strangely it seems that its only a "known problem" among those who are not on it.
Currently Warfarin (brands like Coumadin or Marevan) is the "Gold Standard" for management of Anticoagulation therapy. It is a "narrow therapeutic range drug" which (like sleeping pills) work well with just the right dose: will do nothing if too little and will hurt you if you take too much.
Almost every case of warfarin anxiety I read about in forums about heart related issues follows the same pattern, that is:
- initially afraid,
- started it, nothing happened,
- discovered it was no big deal.
For instance some advice I saw recently posted on a forum for heart valve patients.
"I was very nervous about the drug going into my surgery, and most of it was generated by Google. I think the best advice I could give to someone looking into a surgery would be to disconnect from the internet and listen to your doctors as you ask lots a questions and get lots of answers, as a lot of misinformation and biased information is available at the search engines. I also know that if someone had taken away my internet I would have gone ballistic, so I understand where you are at!"
The medical facts are that if you learn to manage your dose yourself (just like diabetics do, you will test and maintain an INR range)and use a machine (and there are a few on the market) to monitor your INR you will be in a much safer situation than if you rely on a clinic (data presented in a moment below). Yet in the USA the medical establishment (including the medical insurance companies) prefer you to attend a clinic which will most likely use exactly the same machine you would buy yourself (for about $500).
The money facts are that warfarin is a very low price drug (people in the US even buy it at Cosco) and self management is also very cheap. Clearly there is no money to be made in encouraging people down that path. Interestingly the best possible outcome for you is also the cheapest outcome for you.
But its important to remind you that choosing a tissue valve will not mean you are free from anti-coagulation therapy. There is a chance (especially if you are elderly you will be prescribed it for other reasons such as atrial fibrillation).
So (in my view) without mitigating 'co-morbidities' (meaning you're a regular healthy adult), get a mechanical, maintain your INR yourself and live long and prosper.
The risks of taking warfarin are of a bleed or a thromboembolism (clot leading potentially to a stroke).As is stated in the medical literature (and even in this report) the decision of Tissue or Mechanical comes down to balance of choice of tissue valve and its required reoperation or mechanical valve and anticoagulation therapy.
It is this spectre of anti-coagulation therapy which is rattled out by some surgeons (who is it doing the operation again btw?) , with suggestions that anti-coagulation may be as risky as reoperation.
Ok, firstly go back up and re-examine the data on infections ... then consider that the worst possible results from anti-coagulation therapy come from mismanagement of INR. The data on events being poor comes primarially from the results of people who are managed by a clinic rather than who self test. The effective management of INR is not in itself rocket science. Yet the medical system in the United States (where this report comes from) seems to frown upon self testing. This is despite a rather large and growing body of evidence that Patient Self Testing is more cost effective and yeilds better results.
Studies have shown that Patient Self Testing reduced the bleed complications from 11% to 4.5% and Thromboembolic events from 3.6% to 0.9%.
Yet Tissue prosthetic valves are not free from Thromboemolic events nor are the patients free from bleed complications. The article suggests that:
Thromboembolic rates with biologic valves in the aortic position are approximately 0.6% to 2.3% .
So the risk of Thromboembolic rates for Tissue prosthesis is greater than that for well managed INR and Mechanical valves.
On the subject of structural degradation of Tissue prosthetic valves with age The article suggests that:
Observational studies show that the Structural Valve Deterioration rate for current porcine and bovine pericardial bioprosthesis used in the aortic position begins to accelerate after approximately 10 years and continues to increase there after in patients aged more than 65 yearsYet they do not mention how much more rapid this onset of valve failure is in younger patients. And the younger you are the more rapid failure is.
So now, how well does the argument against anticoagulation stack up to you?
With modern western life expectancy as it is (assuming you are 60 or less you have another 20 or more years), why on earth would you choose a tissue prosthetic when you are clearly setting yourself up for another operation in the later years of your life?
Well, one of the reasons I typically read (on heart discussion forums) is that "I want to get over this and go back to my life as it was". Well guess what? Your life will forever be changed by this process (for a start you're alive) and it is generally much better to take the wake-up call and use this as an opportunity to see your life differently. Is taking a pill every day so onerous? Does it make you feel older? Is denial of this worth that much to you?
Of course there are clinical reasons why you may need to choose a tissue prostheses (such as the desire to get pregnant {although I'd have thought that to be reduced in women over 60Yo})
With respect to the initial surgery, the choice of a mechanical valve can make the surgery easier for the surgeon the document states:
Currently available mechanical aortic valve prostheses have several advantages
- ease of insertion,
- safety,
- durability,
- excellent hemodynamics
- long-term track record of performance
- all relatively easy for cardiac surgeons to implant.
- Structural dysfunction of currently approved mechanical heart valves is extremely rare, current mechanical aortic prostheses have endured accelerated bench testing without destruction for the equivalent of several patient lifetimes.
Something else
Money talks (often with the loudest voice), it is commonly said that if you want to understand a business, follow the money. So within that report is the following table (which I suspect has a typo in it)
some things stand out in a quick glance:
- 16,780 valves were mechanical
- 75,734 valves were tissue
- oddly total is also indented under Tissue heading but seems to include Mechanical (although there is a difference when I do the maths VS their Tissue -> Total (I get 507 less)
- Total under Tissue needs to be out dented to match the total of both Mechanical and Tissue.
- Tissue valve costs (I assume this is their cost to the patient, its not mentioned) is $435,716,947 but its not clear if this is tissue valves or all valves and no mention is made of cost per unit between valves.
Lets look at those numbers in another (perhaps clearer) way.
 This means that over 80% of valves sold to 'consumers' in the USA are of the type that will need replacement. In fact its quite probable that some of the valves sold in 2011 were for replacement. Since its quite rare to replace a mechanical valve selling more tissue valves gives greater possibility for then selling another tissue valve. Repeat business is good for business.
This means that over 80% of valves sold to 'consumers' in the USA are of the type that will need replacement. In fact its quite probable that some of the valves sold in 2011 were for replacement. Since its quite rare to replace a mechanical valve selling more tissue valves gives greater possibility for then selling another tissue valve. Repeat business is good for business.Looking at the data sales of valves gives rise to something like $435,716,947 in valves alone. Think of the extra revenue generated in hospital treatments.
That's quite an industry.
On the other and if the consumer (that would be you) got a single operation which gave them a valve that lasted for life where is the business sense in that?
I encourage you to read the guidelines yourself in a careful and critical way. Further I encourage you to read more from trusted sources and most importantly discuss these issues frankly with your surgeon and cardiologist.
Lastly
Ultimately the choice of what valve a patient chooses is significantly up to the patient, unlike buying a washing machine the choice of what valve you choose is something which impacts your life. Do you not owe it to yourself to consider the choice carefully? As the article says:there are few, if any medical procedures that are as effective in relieving symptoms, improving quality of life, and also increasing long-term survival as much as Aortic Valve Replacement for aortic stenosis or aortic regurgitationGiven how the surgery interrupts your life, how anxious patients and family are when this happens, shouldn't you consider the facts carefully? And I mean the facts not the 'stories'.
Anyway, enough about you, think for a moment about your family.
 My wife was distraught at the thought of my surgery (more so than me), she was beside me every step of the way. She said to me in recovery that some of the happiest moments of her life were in seeing me get better every day.
My wife was distraught at the thought of my surgery (more so than me), she was beside me every step of the way. She said to me in recovery that some of the happiest moments of her life were in seeing me get better every day.She put on a brave face, but the fact is that she was scared shitless that I would die and she would be left without me.
She was so pleased because she was so relieved. I would not want to put her through that again. If you are a reasonably healthy adult, and you choose a tissue valve you will for sure be putting your loved ones through it again.
Is that something you want to do to them?



-projections.jpg)












12 comments:
Nicely done. Lots of good information, thanks.
Great article. I have an "old" Starr-Edwards(caged ball) aortic mechanical valve that was implanted at age 31 in 1967(46+ years ago)that is still operating normally. Why any younger person would opt for tissue is beyond me, unless special circumstances exist.
Do you have any statistics on the likelihood of an HAI during valve surgery?
Also, you have an error when you say, "So at 15 years 40% of patients will have had to have their valve replaced for structural degradation." That's only for patients under 40 when they receive a tissue valve.
Anon
Thanks for taking the time to review my post. I had thought the red underlined section directly above it had made that clear. Not clear enough it seems. Thank you for pointing that out.
I have not researched stats on infection from the ohs further thann those stats (which appears to answer your question) as I am still struggling with my infection that I obtained during surgery.
Its a good topic for a post.
I am a MD-Ph-D expert in this particular field since 1978. Your opinion is absolutely right. Marketing is everything and the public is not correctly informed. I could add many clinical and scientific studies that support what you say but are ignored by most cardiac surgeons and cardiologists.
DL. Switzerland
As a patient who has chosen a tissue valve (age 40) I would like to present an alternative viewpoint.
Firstly, having done my research ,both talking to people and looking at peer reviewed papers (and I've spent a LONG time reading Pubmed articles) I note that the experience varies massively with individual personality and sensitivity.
For example - most people get used to the clicking sound, some are "a bit bothered" in the long run and a significant minority (around 5%) really don't like it at all.
If you're like me - someone who is highly strung by nature, and an insomniac who cannot sleep with a ticking bedside clock in the same house - let alone in his head - then mechanical is an awful choice. Even my native heartbeart sometimes sounds loud at night so even a warfarin free mech valve that still clicked would be a awful thing for me to live with.
This is also the case with Warfarin use - there are people very good at controlling it and very happy with it, but also people at the other extreme who absolutely hate it. Their concerns and reported side effects seem to be frequently ignored by their cardiologists, who just insist that they've got the best option.
Secondly, the impact of diet on warfarin is well know. You get people saying "you can eat what you like, you just have to be consistent and adjust the dose accordingly". Well, to me that is most definitely NOT "eating what you like".
I cook with any number of spices that are well known to influence warfarin and the INR - cayenne, turmeric, fenugreek, ginger, the list is nearly endless - and I cook based on intuition, never to recipe. I flatter myself I'm very good at it. Some days, though, I just want bland food with none of the warfarin affecting foods in it. Some days I don't drink beer, other days I like 4 or 5 pints.
Whilst warfarin can be adjusted to a consistent diet. nobody has the ability to predict a different dose every day for wildly varying ingredients that haven't even been measured!
So, if I was maintaining a steady INR, I would have to give up a huge amount of my pleasure and spontenaity in food.
Thirdly, the act of going regularly to a clinic for blood draws - or even home testing - is a constant reminder "you are a patient, you have to be careful", and I freely confess that I loathe being reminded of my condition. I also hate going into hospitals, even though the staff are really nice. Who really wants their self identity to include the words "heart patient"?
Fourthly, I've always been accident prone and quite frequently bang my head on things rather hard. Not a problem at present because I'm rather rugged by nature -used to do martial arts - but potentially risky in the setting of an unstable INR.
Lastly, I am very aware of the latest advances and the potential improvements for tissue valves lifestyle - more durable valves, novel easier to use anticoagulants for those with AFIB (which are contraindicated for mechanical valves), LAAA Occlusion devices, ablation therapy, and other advancements which should have a major impact in reducing the mortality and morbidity for tissue valvers. It should be noted that a lot of compartivie mortality studies are for older generations of tissue valves.
It has been rather difficult to convince my UK cardiologists that my preference is informed - they are incredibly biased towards mechanical valve in the UK, and can't seem to understand why anyone would mind accepting this for the rest of their life, with no hope of it getting better.
I should also add that I have no truck with the idea of counselling, the "if you can't change something, let's manage how we feel about it", whilst I freely admit that others will benefit from it.
Fortunately the surgeon about to do my operation listened to my reasons and said "You have cogently and clearly expressed why your preference is for tissue, and I respect that".
One size does not fit all
Hi Andy, thanks for your comment. Definately 1 size does not fit all, and I think I have not tried to say it does.
Many tissue valve recipients however do seem to take such a view and its interesting to hear that in the UK cardiologists take the opposite view as seems to be the case in the USA.
Personally I've had a repair, then a homograft then a mechanical.
You say: "So, if I was maintaining a steady INR, I would have to give up a huge amount of my pleasure and spontenaity in food"
This is simply not the case with everyone (or in my findings most people). When it comes to warfarin if you have not been on it and managed it yourself I think that you just can't make a statement about how eating and drinking will effect it. You can read this and that but essentially you will not be as informed about how it will work because the literature mushes up everything into stats without the capacity to compare between groups.
I eat and drink what I like and I'm in range 98% of the time with weekly measurements.
My Best Wishes to you
Also Andy you say:
"I freely confess that I loathe being reminded of my condition."
I hope you move past this some time in the future, for it is just denial. You will never be past this as all the treatments have issues one way or another. There is no "Cure".
To quote from an old movie: you have to make a friend of horror, for if you do not make a friend of horror, then horror is an enemy, an enemy be truly feared.
Personally I have always tried to make my decisions free from fear.
again, my best wishes for your future good health.
Thank you for this detailed review. I'm about to have an AVR in a couple of weeks, and I chose to go with an On-X mechanical valve. However, today I came across a chart (link below) that shows that the life expectancies of people who have had AVR are significantly lower than the general population, regardless of tissue vs mechanical. My symptoms are not too bad and I may be able to wait a few years. What's your take on this study? If this is true, would it make sense to hold off on the surgery as long as possible, without causing any permanent damage to the heart?
Link to the chart:
http://www.jtcvsonline.org/cms/attachment/2005364699/2023154440/gr1_lrg.jpg
Link to the full article:
http://www.jtcvsonline.org/article/S0022-5223(08)01572-9/fulltext
Hi
well first I'll speak to your point of:
> if this is true
Of course its "true" ... its in a peer review journal. However true or false is simplistic, the crux of the matter is more complex. For instance a cone is a triangle from the side and a circle from the bottom. Arguing if its a triangle or a cone and which is true is not meaningful.
So with that in mind lets look at the question you've asked about delaying surgery. There is nothing in that article which speaks to that. It does not mention delayed surgery from diagnosis, it just discusses ages. So for all you know (and I would suspect this to be an aspect) the longer people waited from diagnosis to surgery (despite their age) the worse the outcome was for them and contributed to the lower than "general population" life span.
In short this article does not suggest anything like your question of holding off surgery.
Further the article does not mention any detail (they seldom if ever do) about the cohort under study and we do not know what their general condition was like or what other health problems they had. I've had a cousin with a heart issue similar to me. He was dead years before my age because his very excessive drinking and dreadful diet, combined with his total disinterest in taking care of his health played a very real role in shortening his life. The data makes no discussion of the details.
So that means that the differences in ages in that graph are more or less guidelines to the general population. Are you "average"?
Next the graph does not show "error bars" indicating the ranges. For instance if aged at 55 the graph would suggest life expectancy is around 15 ~ 17 years for someone who had had an AVR but 25 for general population. Clearly some of the general population lived longer and some less. Same for the valvers. So by how much and it is quite possible that some had valves done and lived longer than some of the general population.
Do you begin to see that its not just as simple as lines?
Then there is a great question in my mind of "why does the BC population live so much longer than US or UK? Is this diet related? Lifestyle?
Lastly the data is old: patients between 1982 and 2003 and things have moved on in post operative care as well as how people act after surgery. Do not live "in cotton wool" if you want to live longer.
So to me I feel you should get the surgery done earlier than later. It is emerging in the 'literature' that the older school view of waiting till you're at greater risk of dying than surgery is stupid, especially when you are sure you will need the surgery. By being younger and healthier you will make a better recovery. I can assure you that when I had my surgery done at 28 I had run down a lot before the surgery and so it took years of hard work to get fit again.
That's my 10c
Best Wishes
lots of information i get here good shearing brother
1) I have no family
2) I am a lifelong insomniac, depressive, lots of anxiety and have had full blown reactive tinnitus and hearing loss for 26 years so I dread the ticking as well but also dread future surgeries from a tissue valve----
Post a Comment